Deep Vein Thrombosis (DVT) - Medical Notes
By Dr Nehana Gittens (FY2)
A venous thrombus embolism (VTE) is a blood clot that forms in the venous circulation. The clot can then disrupt blood flow which can become life-threatening and potentially fatal. The types of VTE include deep vein thrombosis (DVT) and a pulmonary embolism (PE).
Click here for our article on PE.
DVT (Deep Vein Thrombosis)
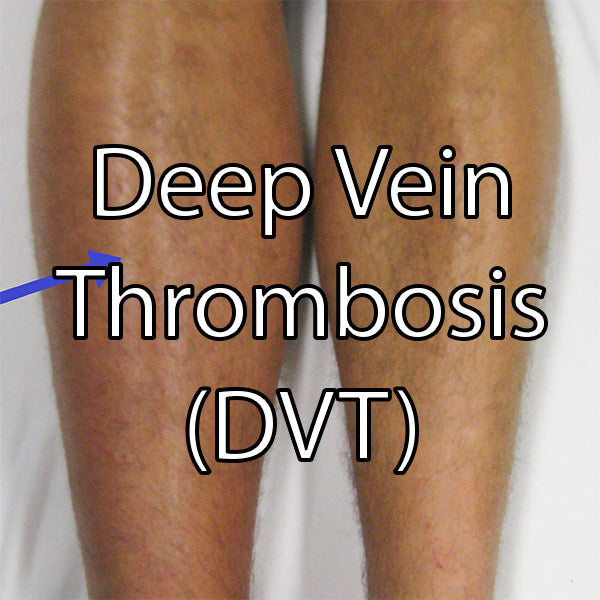
This occurs when a blood clot develops in the major deep veins. It commonly occurs in the leg, thigh, pelvis or abdomen, but can occur less commonly in the arms, or portal system. This article will focus on DVT in the lower extremities. DVTs can cause pulmonary embolisms which can be fatal.
Signs/Symptoms
- Unilateral
-
Calf swelling
- >3cm difference between calves
- Measured from 10cm below tibial tuberosity
- Painful (localised along deep venous system)
- Asymmetric pitting oedema
- Prominent superficial veins
- Colour changes to leg e.g red, purple/blue mottled

Understanding Risk Factors for DVT
To understand the risk factors for DVT it is useful to understand Virchow’s Triad.
This is a triad of factors that increase the chance of a blood clot forming by stimulating activation of the clotting system.
The Three Factors:
- Hypercoagulability of blood
- Stasis of blood flow
- Vessel wall injury

The effect of these factors on blood flow can increase blood coagulation. Risk factors (located below) for clotting fall under these major factors for clotting, such as immobility which causes stasis of blood flow.
Risk Factors
- Immobility
- Recent surgery
- Long haul travel
- Malignancy
- Pregnancy
- Thrombophilia e.g antiphospholipid syndrome, Factor V Leiden
- Hormone estrogen therapy
- Trauma
Investigations
When a DVT is clinically suspected a Wells Score for suspected DVT is calculated (click here for a calculator from MDCalc) This gives an indication as to whether a DVT is likely or not.
D dimer
- This is a blood test for protein in blood when clots dissolve
- It is sensitive not specific; can be raised in other conditions e.g infection
- Rules in an DVT but does not confirm it
USS Doppler
- Scan of venous system to identify a clot
- Definitive investigation
Further Investigations
- Bloods: FBC, U&Es, LFTs, clotting
- CT (in some cases)
Management
DVTs are treated with anticoagulation. Treatment dose anticoagulation is recommended to be started immediately when VTE is suspected. DOACs are more commonly used first line such as apixaban or rivaroxaban. Alternatively, LMWH (low molecular weight heparins) can be used e.g enoxaparin.
Dosing example of apixaban for DVT:
- 10mg BD for 7 days (loading dose), then 5mg BD till the end of therapy
Length of Treatment
- 3 months → patients with identifiable/reversible cause of VTE
- 3-6 months → patients with active cancer
- Long-term → patients with unprovoked VTE, recurrent VTE or an irreversible underlying cause e.g thrombophilia
Extra Tips – DVT vs Cellulitis
Sometimes DVT and cellulitis (infection of the skin) can present similarly. It is important to differentiate between them as they have different management pathways.
DVT and Cellulitis Similar Symptoms
- Swollen leg
- Erythema
- Painful
- Warm
- Acute onset
What makes cellulitis more likely?
- Signs of infection - typically hot, shiny and tight, can be blistering
- Site of entry - skin breaks? cuts? insect bites?
- Systemic illness - fevers, chills, malaise

Image credits
Image of DVT affected leg: James Heilman, MD, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons
Image of Virchow's Triad: Rudolf.hellmuth, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons
Left cellulitis of leg: Stephen Ewen, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
References
- BMJ Best Practice. (2024). BMJ Best Practice VTE. Available at: https://bestpractice.bmj.com/topics/en-gb/3000201/treatment-algorithm (Accessed: 18 February 2024).
- NICE. (2020). Oral anticoagulation prescribing in DVT and PE. Available at: https://cks.nice.org.uk/topics/deep-vein-thrombosis/prescribing-information/oral-anticoagulants/ (Accessed: 21 February 2024).





Leave a comment